Our 2024 Legislative Priorities
Several important pieces of legislation have been introduced in the current Congress, and we are actively working to enact these bills that would affect kidney patients and their access to life-sustaining health care.

The Living Donor Protection Act of 2023 (H.R.2923 /S.1384)
Introduced by Representatives Jerrold Nadler (D-NY) and Greg Murphy (R-NC) and Senators Kirsten Gillibrand (D-NY) and Tom Cotton (R-AR), the Living Donor Protection Act would remove many barriers to living organ donation by ensuring that living organ donors have Family Medical Leave Act (FMLA) protections and protection from discrimination by insurance carriers.
This bipartisan bill would codify a 2018 U.S. Department of Labor letter which stated that organ donation is protected under FMLA so that donors are able to take time off of work to donate their kidney and recover from surgery without fear of losing their job. It also prohibits insurers from:
- Declining or limiting coverage of a person under any life insurance, disability insurance or long-term care insurance policy due to the person's living donor status;
- Preventing a person from donating all or part of an organ as a condition of receiving a life insurance, disability insurance, or long-term care insurance policy; and
- Taking a person's status as a living organ donor into consideration when determining the premium amount.
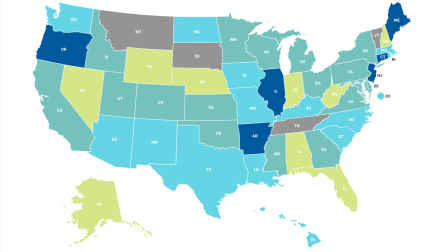
Finally, the bill requires the Department of Health and Human Services to update its website, brochures, and other media regarding live donation and access to insurance for living donors. Check out the American Kidney Fund's State of the States: Living Donor Protection Report Card to see how well laws in your state encourage living organ donation and reduce barriers for living organ donors. If passed, this federal legislation would ensure that every state has a basic level of protection, so that a person's state of residence does not make it more difficult to be a living donor.
New Era of Preventing End-Stage Kidney Disease Act of 2023 (H.R. 6790)
There are about 150 rare kidney diseases, and no FDA-approved treatments for most of them. Many rare kidney disease patients struggle to receive an accurate diagnosis and expert treatment. These treatment and diagnostic barriers, coupled with the lack of rare kidney disease awareness and education, often cause a delay in diagnosis. This delay can result in a rapid decline in kidney function and, ultimately, kidney failure when the only options are dialysis, transplant, or death.
Each day in the United States, on average, 360 people begin dialysis, and 13 die waiting for a kidney transplant. In 2019, Medicare spent a total of $124 billion on chronic kidney disease (CKD) and ESRD. Additionally, communities of color are disproportionately affected by rare kidney diseases and a lack of adequate treatment options due to existing health disparities — Black Americans are 4-5 times more likely to develop kidney failure than white Americans.
To address rare kidney disease in the United States, we need more research, public awareness, shorter times to diagnosis, access to genetic testing and counseling, additional treatments, and an understanding of why rates of kidney disease are higher in underserved communities. These steps would help assuage the burden of rare kidney disease on individuals and help defray the costs of dialysis and kidney care in the Medicare program.
The New Era of Preventing End-Stage Kidney Disease Act of 2023 will be introduced by Congressman Gus Bilirakis and Congresswoman Terri Sewell. The bill aims to improve the understanding and timely and accurate diagnosis of rare kidney diseases. Please email your elected officials today to request they become an original cosponsor of this important bill.
Click here to contact your United States Representative and ask they cosponsor this important legislation.
Restore Protections for Dialysis Patients Act (H.R. 6860)
For over 40 years, end-stage renal disease (ESRD) patients on dialysis have had the option to retain their employer group health plan or COBRA coverage for up to 30 months before moving to Medicare as their primary insurance as part of the Medicare Secondary Payer (MSP) law. Specifically, the MSP provisions protect ESRD patients from discriminatory practices by insurers that would discourage their enrollment in a private plan.
However, in a recent U.S. Supreme Court case, the MSP law was interpreted in a manner that would allow plans to get around those protections for ESRD patients and undermine Congress's intent in adopting them.
H.R 6860, the Restore Protections for Dialysis Patients Act, is bipartisan legislation that would clarify that insurance companies comply with the Medicare Secondary Payer law by specifically stating that a health plan cannot discriminate against dialysis patients by providing less dialysis services compared to services for other chronic illnesses. It will ensure that dialysis patients have access to the care they need on their employer sponsored insurance for 30 months before moving to Medicare as their primary insurance.
Please contact your United States Representative and ask they cosponsor this important legislation.
Chronic Kidney Disease Improvement in Research and Treatment Act (H.R. 5027/S. 4469)
Introduced by Congresswoman Carol Miller (WV-1) and Senator Ben Cardin (MD) this bill aims to improve the lives of those with kidney disease. The legislation would increase awareness of kindey disease and expand preventative services.
Specifically, among other provisions, the bill would:
1) Include Kidney Screening in the Annual Medicare Wellness Benefit. Many people with kidney disease do not know that they have it. Including a screening in the yearly wellness checks for Medicare beneficiaries will provide patients and their doctors with a report of kidney function. It will allow doctors to track if kidney function decreases over time and provide early interventions.
2) Expand the Medicare Kidney Disease Education (KDE) benefit. The KDE benefit is a service covered by Medicare. At stage four of chronic kidney disease (CKD), Medicare recipients can meet with a doctor to learn about CKD and how to improve health to delay dialysis. It can also include information on nutrition, the importance of exercise, management of other chronic diseases like heart disease or diabetes, and treatment modality options such as in-center hemodialysis, home dialysis, and kidney transplant. The bill would expand the benefit to allow dialysis facilities to provide this information. It would also expand the number of health care providers reimbursed for this information to include physician assistants and nurse practitioners. The bill would also allow patients with stage 5 CKD to access the KDE benefit.
3) Expand Access to Medigap plans. Medicare beneficiaries under 65 are not guaranteed access to a Medicare supplemental plan called Medigap. Medicare Part B pays 80% of dialysis costs, and the patient must pay 20% with no out-of-pocket cap. Medigap plans cover the portion that Medicare does not cover. The state regulates Medigap for people under the age of 65. Eighteen states do not require Medigap insurers to offer Medigap to ESRD patients under age 65. The bill would require all ESRD patients with Medicare to be guaranteed access to a Medigap plan regardless of their state. The provision would ensure that more dialysis patients have the full health insurance coverage they need.
4) Study on How to Increase Kidney Transplants. The bill would require the Secretary of Health and Human Services (HHS) to submit a report to Congress on how to increase kidney transplants. The study would report on possible economic disincentives in the Medicare program, practices used by states with higher than average transplant rates, barriers to increasing living donation, and deceased donations.
5) Expanding TDAPA to Medicare Advantage (MA) Plans. Currently, the Transitional Drug Add-On Payment Adjustment (TDAPA) and Transitional Add-on Payment Adjustment for New and Innovative Equipment and Supplies (TPNIES) do not apply to drugs and devices taken by dialysis patients enrolled in MA. The bill would provide increased payment adjustments to providers or facilities when the drugs and devices covered under TDAPA and TPNIES increase the cost.
6) Increasing Payments to Providers to Account for Increased Labor Costs. The bill would require the Secretary of Health and Human Services (HHS) to calculate accurate costs when deciding on the annual payment increase for kidney care providers.
Please contact your U.S. Senators and Representatives.
The Kidney PATIENT Act (H.R. 5074)
Oral-only drugs used for the treatment of end-stage renal disease (ESRD) are covered under the Medicare Part D prescription drug benefit. However, the Centers for Medicare and Medicaid Services (CMS) has indicated that it will start including oral-only ESRD drugs in the ESRD Prospective Payment System (PPS), also known as the "bundle," starting Jan. 1, 2025. CMS had planned to implement this change earlier, but Congress previously stepped in and passed legislation delaying when CMS could make this change to how oral-only ESRD drugs are covered in Medicare.
Phosphate-lowering drugs are oral-only medications taken by most people on dialysis, and there are many types of phosphate-lowering drugs that work for different patients. Moving coverage of oral-only phosphate-lowering drugs to the ESRD payment bundle would create access issues for patients taking these critical drugs. There would also be logistical challenges for ESRD facilities that would now be responsible for acquiring, storing and distributing these drugs, of which there are many types and many patients prescribed them. Additionally, patients take phosphate-lowering drugs multiple times a day with meals and snacks, so the quantity of pills also contributes to the logistical challenges.
With the new beneficiary out-of-pocket cap in the Medicare Part D program and the expanded eligibility for the low-income subsidy, the affordability of Part D drugs is further enhanced. Keeping coverage of oral-only ESRD drugs in the Part D program makes sense in terms of patient affordability and maintaining patient access to treatments.
The Kidney PATIENT Act (H.R. 5074) is bipartisan legislation that would delay the move of oral-only ESRD drugs into the ESRD bundle until 2033 or until new intravenous therapies come to the market. The bill would ensure patients have access to the medications they and their doctors have determined work best for them. In addition, the bill would save money for taxpayers because it would delay an increase in the ESRD base rate that determines the bundled payment that would occur when adding oral-only drugs to the bundle.
Please ask your member of Congress to support the Kidney PATIENT Act.
Access to Genetic Counselor Services Act of 2023 ( H.R. 3876/ S. 2323)
Chronic kidney disease (CKD) is one of the leading causes of morbidity and mortality worldwide and a significant number of cases are from an unknown cause. The American Kidney Fund is working to help identify why so many patients get CKD, and genetic counseling has a powerful role to play in that endeavor.
Genetic counselors are trained and certified to interpret complex genetic information and share that information in an understandable way with patients. Currently, Medicare does not recognize genetic counselors as healthcare providers, which can leave kidney patients without access to a professional who can help them understand how their genetic makeup could impact their health or influence their choice of treatments.
The Access to Genetic Counselor Services Act of 2023 (H.R. 3876/S. 2323) would change Medicare law so the program would recognize genetic counselors as healthcare providers so they can be reimbursed directly by Medicare. The bill would give Medicare beneficiaries greater access to their services.
Requiring Medicare to recognize genetic counselors as providers also has an impact on private insurance. Some insurers do not cover services from a provider not recognized by Medicare, which can lead to high out-of-pocket expenses for patients requiring the services of a genetic counselor. This makes pursuing the needed medical knowledge, information, and treatment plan very difficult and it comes at a time when families are facing complex medical decisions.
Please contact your U.S. Representatives today.
PASTEUR Act of 2023 (H.R. 2940/S. 1355)
Superbugs are infections resistant to antibiotics; when these ailments do not respond to medicines, they are called antimicrobial resistance (AMR). In 2019, 5 million people worldwide and 173,000 deaths in the United States died from AMR-associated issues.
AMR is even worse for dialysis patients because they are particularly susceptible to infections. The Centers for Disease Control and Prevention (CDC) reported that people on dialysis are 100 times more likely to develop a staph bloodstream infection compared to those not on dialysis. Unfortunately, there has been a lack of innovation in antibiotic drugs. The last new class of antibiotics came to market in 1984. Pharmaceutical companies could only bring 12 new antibiotics to patients in 2017 and 2021. More needs to be done to address AMR.
In April 2023, a bipartisan group of Senators and Congressmen introduced the Pioneering Antimicrobial Subscriptions To End Upsurging Resistance (PASTEUR) Act. The bill aims to increase the number of antibiotics and prioritize new, more potent medicines that can treat severe infections.
The PASTEUR Act would specifically:
Create a "Committee on Critical Need Antimicrobials," comprising federal agency officials, doctors, patients, and experts. The committee would decide which infections are of most concern and what properties the potential drugs should possess. Establish a "Subscription Model," providing companies with up-front funding and a regular subscription payment to develop the new drugs. In return, the companies would give access to these drugs to patients. Expand data collection and reporting on antibiotic use, resistance, and patient outcomes data through the CDC National Healthcare Safety Network.
Please contact your U.S. Senators and Representatives.
CARING for Social Determinants Act of 2023 (H.R. 1066)
Kidney disease affects communities of color at higher rates than the white community. Due in part to high rates of diabetes and high blood pressure — the two leading causes of kidney disease — communities of color have disproportionately high rates of kidney failure. For example, Black Americans make up 13% of the U.S. population but account for about 35% of Americans with kidney failure. Additionally, Hispanic people in the U.S. are twice as likely as white people to develop kidney failure.
One way to address these health disparities is to address social determinants of health (SDOH) – the conditions.
The Centers for Disease Control and Prevention (CDC) defines social determinants of health (SDOH) as "conditions in the environments where people are born, live, learn, work, play, worship and age that affect a wide range of health, functioning and quality-of-life outcomes and risks. These determinants can have a major impact on people's health and well-being.
Essentially, there are correlations between non-medical factors and poorer health outcomes. There is an association between a healthy community and access to nutritious food, safe housing, education, and good jobs.
As part of the CDC's Healthy People 2030 initiative, they included a goal of creating "social, physical, and economic environments that promote attaining the full potential for health and well-being for all." The CDC has stated that community-wide, nonclinical aspects of public health show positive outcomes that improve public health and decrease health care costs.
As part of efforts to address SDOH, Reps. Lisa Blunt Rochester (D-DE) and Gus Bilirakis (R-FL) introduced H.R. 1066, the CARING for Social Determinants Act of 2023. The bill would require the Centers for Medicare & Medicaid Services (CMS) to provide guidance every three years to each state to address SDOH through Medicaid and the Children's Health Insurance Program (CHIP). In many states, private health insurance companies referred to as Medicaid managed care organizations (MCOs) provide health benefits to Medicaid and CHIP beneficiaries. They have innovative ideas and use their funding to help beneficiaries with nutrition, housing, or caregiving. These programs can be replicated in other states. Providing this information to Medicaid and CHIP programs in other states can provide state leaders with the knowledge to utilize those ideas in their states. It can help address underlying issues that lead to higher rates of diabetes and hypertension, and thus, higher rates of kidney failure in underserved communities.
Click here to contact your U.S. Representative.

AKF allowed me to focus on my health and prioritize my new kidney. I didn't have to worry about how I was going to pay for my insurance. They had my back when I needed it.
— Alysia Yamasaki

Where Americans live can affect their ability to give the gift of life
AKF's State of the States: 2025 Living Donor Protection Report Card evaluates each state and the District of Columbia on how well their existing laws encourage living organ donation and reduce barriers for living donors.