Pediatric lupus nephritis

- Medically reviewed by
- Gina-Marie Bartletta, M.D.
- Last updated
- September 25, 2023
What is pediatric lupus nephritis?
Lupus nephritis in children is called pediatric lupus nephritis. Up to 20% of people with lupus (1 in 5) were diagnosed as children or teens, and lupus nephritis is common in children with lupus.
Lupus nephritis is more common in children diagnosed with lupus than in adults with lupus. Lupus nephritis occurs in around 50–82% of children with lupus in comparison with 20–40% of adults with lupus.
What causes pediatric lupus nephritis?
Doctors are not sure why some children have lupus and others do not.
Lupus can run in families, but many children who have a relative with lupus do not get it themselves.
Doctors think some children have genes that can make their chance of getting lupus higher. Certain triggers can cause these children to develop lupus, such as:
- Infections
- Viruses
- Toxic chemicals or pollutants
How does lupus nephritis affect young people?
Symptoms for pediatric lupus nephritis are similar to the symptoms adults may have. However, if your child has lupus, it may be more likely that your child's organs have been affected or damaged. These effects may include kidney, lung, or brain inflammation.
Signs of kidney inflammation (called nephritis) may include:
- Bloody urine
- Foamy or bubbly urine (sign of too much protein in the urine)
- High blood pressure
- Swelling of the face, abdomen, legs, ankles, and/or feet
- Weight gain Signs of lung inflammation (called pleuritis) may include:
- Shortness of breath
- Sharp and stabbing chest pain that is worse when you take a deep breath or cough
Signs of brain inflammation (called cerebritis) may include:
- Headaches
- Memory loss
- Problems with hearing, speech, vision, or movement
- Changes in behavior or personality
If your child has any sudden and drastic changes to their health, seek medical care right away.
Who can get pediatric lupus nephritis?
Only young people who have lupus can develop pediatric lupus nephritis.
Pediatric lupus is more common in young people who have already entered puberty, and is more common in adolescent (around ages 12 – 17) girls than boys. For children who have not yet started puberty, it is only slightly more common in girls than boys.
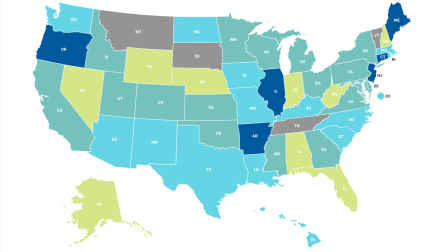
Similar to lupus in adults, children of racial or ethnic minorities, such as African Americans, Hispanics, and Asian Americans, also have a higher chance of getting lupus.
What is the outlook for children with lupus nephritis?
The outlook for pediatric lupus has improved over the years. A study from 2012 showed that children with lupus are highly likely (85%) to survive more than 10 or 15 years after their diagnosis. However, despite advances in treatments for lupus nephritis, the rate of complete remission, which is the disappearance of the signs and symptoms of a disease remains suboptimal and long-term survival appears to have leveled off over the past few decades.
Current long-term follow-up studies suggests that up to 3 in 20 children (15%) with lupus nephritis will progress to end-stage renal disease (ESRD) — which is when kidneys are no longer able to function well enough for day-to-day life. If an individual with lupus nephritis develops ESRD, the outcome can be quite good with kidney transplantation, as there is rarely recurrence of lupus nephritis in the new kidney.
Kidney transplant survival is like that seen in transplant patients without lupus, with 5-, 10-, 15-, and 20-year kidney transplant survival of 81%, 79%, 57% and 51%, respectively.
How can my child and I cope with pediatric lupus nephritis?
Having a child with a chronic (long-lasting) illness can affect your whole family. It is important to:
- Explain to your child and other family members what is going on
- Tell your child how lupus nephritis may affect their day-to-day life
- Be your child's advocate
- Provide comfort and support for your child
- Seek out a pediatric nephrologist (kidney doctor) along with a pediatric rheumatologist (lupus specialist)
It may be a good idea to look for a mental health therapist for you and your child to help you through a pediatric lupus nephritis diagnosis
What should I know about transitioning from pediatric lupus nephritis treatment to adult treatment?
As children get older, they will start seeing adult health care providers instead of pediatric or child focused providers. For some, this happens after high school, for others it may not happen until they are in their twenties. Regardless of when it happens, this change presents many health and social challenges, especially for young people with lupus and lupus nephritis.
What can I expect when transitioning to adult care as a young person?
As a young person with lupus, this transition can be especially challenging as you get ready to leave the health care providers you may have known for a long time. It's important to remember that lupus is a life-long disease, so learning how to manage your symptoms and care can allow you to live a long, healthy life.
Here are some common challenges that people face while switching to adult care along with some strategies to cope with them.
Medical Challenges
Maintaining or changing health insurance
- Insurance can be intimidating and there's often more questions than answers.
- Talk with your insurance provider early on to understand what might change as you switch care providers, and work with your parents or caregivers to remain either in network or with a provider that your insurance will accept.
- Changes to insurance can result in gaps between appointments and medication refills.
- Ensuring that you continue to get the care you need is crucial to your health. Work with your health care providers to create a backup plan in case you experience a gap in care.
- If you live in the US and receive dialysis for end stage renal disease you may qualify for American Kidney Fund's Health Insurance Premium Program (HIPP), which provides financial assistance for people who cannot afford their monthly insurance premiums.
Progression of kidney disease
- Lupus nephritis occurs in 50% of people with lupus and many will experience kidney failure, particularly those that developed it during childhood.
- Stick to your medicine routines, track your symptoms, and communicate with both your pediatric and adult health care providers about any changes to help prevent further kidney damage.
- It can be easy to go a while between appointments during a transition period. However, symptoms of kidney disease are not often felt, so it's crucial to keep all appointments and stay on track. There is no cure for kidney disease, but you can prevent further damage from being done.
Social challenges
- Anxiety in switching providers - You've probably been with the same providers for a long time, maybe since you got diagnosed. It's normal to feel nervous or sad when thinking about having a new team. You can take steps to encourage communication between both teams and build relationships with your new providers.
- Ask your current health care provider for a referral to doctors working with adults, this could be from your current nephrologist (kidney doctor) or rheumatologist (doctor with specialized training in inflammatory diseases).
- Check-in often with both your new adult team and your previous pediatric team to make sure information is being shared and your concerns are being heard.
- Don't be afraid to express how you feel or ask questions of your family and/or care team. Open communication can help them support you.
- Lupus can disrupt activities of daily life like school or work. The transition to an adult provider is likely happening during other major transitions in your life, such as graduating high school and getting ready for college or a job. Your experiences will probably look different than your peers, and it might feel isolating. Appointments, symptoms, and medicine might mean that you can't attend work or school. It's important to talk to your support system about how you're feeling. Your mental health is a part of your physical health.
What can I expect as my child transitions to adult care?
As a parent or caregiver, you have probably grown used to being the "driver" of your child's care. You may make appointments, provide transportation, help with medicine management, and many other aspects of care. As the transition from pediatric to adult care begins, your child will start to become their own driver. Many people in this position have reported struggling with this transition, and these feelings are valid. However, it's important to be supportive and active in this transition so your child continues to have the greatest chances at success.
Here are some challenges you may face and some strategies to cope with them.
Challenges Faced by Parents and Caregivers
Feelings of losing control are normal, but working with your child to build their independence can help ease this feeling. It's important for your child to become independent and learn to manage their own care. You can act as a role model and demonstrate proactive behaviors for them. Here are some suggestions:
- Involve your child early. Studies have shown that children who are educated about their disease, medicines, and symptoms early on have better health outcomes.
- Make appointments and keep track of them on a calendar that they can easily see. As they get older, encourage them to make their own appointments.
- Include them in their medicine management such as setting up a pill organizer, taking them to the pharmacy and using full medicine names.
- Ask them if they have any questions for the doctor prior to appointments and write them down.
Issues with insurance
You or your family may be a source of insurance for your child. As they switch providers or get their own insurance plan complications will likely arise. Be prepared for this by reviewing details of your plan in advance and being a resource for your child for any questions they might have.
How can my family prepare for the transition?
Changing providers is a major change for patients and families. Together, you can help make it a smooth transition.
Here's a list of strategies:
- Take time to reflect individually. Some questions to ask yourself are: What feelings are coming up for you as you navigate these new changes? What are you concerned about? What questions do you have for the old care team? The new care team?
- Make a plan together.
- Consider drafting a timeline of the transition with an end date in mind.
- Ask your pediatric provider for a list of recommended doctors and make a few appointments before deciding anything. You can "interview" more than one doctor to find the best fit.
- Write out a list of questions for both the pediatric and the adult health care providers and make sure the two teams are communicating.
- Set time aside to do things outside of managing the transition. Go for a walk, listen to music, take a trip, or watch a movie together. It's important to create time to care for yourselves.
Learn more about the transition of care from pediatric lupus nephritis treatment to adult care.